Focus on wellbeing: A tale of two professions in occupational supervision
“What makes you qualified to work with people in professions that you know nothing or little about?” I was faced with this challenging question recently; it is the type of question I welcome because it opens an opportunity for discussion.
 As an occupational supervisor I enter supervision as a space of not knowing, to focus on the experiences of the supervisee, without evoking any memories from my experiences or beliefs. Referencing my own experience would impede creative thinking and interfere with the process. If you like, going into my “filing system of experiences and knowledge” to support the supervisee in the same way as a coach or learning mentor.
As an occupational supervisor I enter supervision as a space of not knowing, to focus on the experiences of the supervisee, without evoking any memories from my experiences or beliefs. Referencing my own experience would impede creative thinking and interfere with the process. If you like, going into my “filing system of experiences and knowledge” to support the supervisee in the same way as a coach or learning mentor.
Viewing supervision as a reflective process allows participants to think deeply and vulnerably about all aspects of life, particularly if it has an impact on work. Being vulnerable and reflecting can be challenging for many professionals, who can never afford to appear as less than efficient and effective.
As the supervisory relationship develops and facades are lowered, we begin to discuss deep emotions and long-held ideas that colour our thinking and behaviours, drawing parallels between past, present and environmental factors.
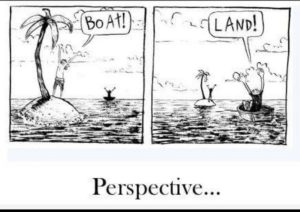 What I offer during discussion is perspective from another viewpoint, a naïve viewpoint that sees the situation without all the weight of responsibility or prejudice. I call this “island hopping”, where the dilemma looks different from my vantage point. We consider patterns of practice or thinking and the typical results these have delivered in the past.
What I offer during discussion is perspective from another viewpoint, a naïve viewpoint that sees the situation without all the weight of responsibility or prejudice. I call this “island hopping”, where the dilemma looks different from my vantage point. We consider patterns of practice or thinking and the typical results these have delivered in the past.
For obvious reasons then, I cannot do this if my experiences are too like theirs: there needs to be cognitive distance, unlike clinical supervision where the supervisor imparts their wisdom gained through long-term experience.
There are familiar patterns seen in a few professions, none more so than in medical and legal practice. Both adhere to codes of practice that I familiarise myself with before we work together. Both are considered well respected and desirable careers, held in high esteem in western culture.
 But we cannot overlook how this came about, so we need to step back in time.
But we cannot overlook how this came about, so we need to step back in time.
History binds these two professions in many aspects, particularly the theatrical nature seen in the infancy of medicine and law.
The scene was set for outpourings of adoration (so long as they were “winning”), unfathomable respect (including investiture), proffering enlightened thinking drank in by spectators who paid to witness such greatness.
The foundations were laid for those who came after to constantly attempt to reach a sometimes unobtainable bar.
Little wonder then that today there is a hangover of pressures bestowed upon legal and medical professionals that still haunts, albeit to a less degree. Perfectionism is commonplace; in occupational supervision we investigate if this extends to all areas of life, which all too often it does, affecting intimate relationships.
Today the drive to enter either profession is often claimed to be to help those in need. However, qualifying and attaining higher roles in these professions comes at a cost. From the outset competition faced to secure a place at university is fierce, the student often forgoes certain freedoms peers may enjoy. Commonly seen is parental pleasing, following in their parents’ footsteps or achieving their parent’s dream so they can bask in the glory of their child’s achievement.
How this plays out in supervision for both legal and medical practitioners is typically seen as a mixture of delight and frustration. It impacts on ideas of self and role with family and the workplace; it fosters a sense of duty.
Of all the professionals I see, the two types that identify closest to their role in the workplace are legal and medical practitioners. Equally, both profoundly fear losing their identities as lawyers or medics – it becomes an extension of who they are. Both, however, find their concerns fade as a result of entering reflective practice. Revealing authenticity in a human-to-human encounter.
“Come to the edge Life said/ They said: We are afraid.
Come to the edge Life said./ They came. It pushed them…
And they flew” (Guillaume Apollinaire)
In occupational supervision, who we are and how we operate are key components of our exploration.
Well trained supervisors will have extensive knowledge of theory and tools to work safely and ethically. We rely on fully understanding the dilemma of being a human that can often clash with the role we play as the professional, and how we present from who we are to how we are in the supervisory relationship. Most supervision adopts the well-respected Seven Eyed model of supervision, to map out what takes place and how the focus shifts from the supervisee to the supervisor and eventually the wider context of the organisation in which the supervisee works, sometimes even as wide as global conditions.
Through my experience of working with barristers and medical consultants, as well as knowledge that is documented in research, I can attest typical concerns that are shared in supervision. For the sake of ease I will relate examples to barristers and medical consultants.
Typical issues which arise that impede practice are, primarily, fear of failure both in procedure and in personal limitations. When we consider that clients’/patients’ lives can be changed for better or worse in their hands, this is not surprising. However, both see failure as shameful and stigmatising.
It does not come as a surprise then that both enjoy (some more than others) praise when it is given. “Winning” is seen as very important – it means the practitioner will maintain expectations and often lack focus on their mental wellbeing. Secondly, then, is a drive to work harder even when energy is low. On exploring the purpose and meaning of winning or getting things right, we arrive back at the reason for choosing this profession in the first place. A result of such pressure is seen in high rates of dysfunctional behaviour, such as addiction.
The Seven Eyed model requires us to look at self, how we were in the moment and if that had an impact on how we viewed what took place. When asked to describe entering the office/courtroom or ward/operating room both notice changes in behaviours of others in activity and productivity. Nurses dash about looking busy or holding relevant notes in preparation. Lawyers announce the barrister has entered the building, the boardroom/consultation room is fully prepared. Their “audience” awaits their expertise, skills, and ways in which they interact with clients/patients exuding charm and efficiency. They enter a persona expected of them, designed to play their role in gaining the best possible outcome for their client/patient.
All the professionals I have worked with claim to have been high achievers in school, meaning for them working hard is expected and a way of life, they invest a large amount of time into the work they do.
They do not respond well to criticism or complaints. Added to responsibilities and difficulties they face are patients who have googled their issues so tell the consultant what they need and how to do it. Clients have either had previous experience or have a “friend” who knows what needs to happen and what outcome they see happening in court proceedings. Neither of whom account for the restricted paths of intervention or process dictated by the NHS or the law/judge’s decision.
In supervision we look at meaning, we reflect on our thinking and what happens to us and even where we go in our minds. An example of this might be entering into the situation together by asking the supervisee to describe what happened, who was there and what they anticipated to unfold.
Both have revealed difficulties in leaving their professional role when they are not in work. Or how work has impacted on intimate relationships. In entering the process of preparation for going to court or preparing for surgery I enter the space with them, curiously. I ask how this feels for them, what is going through your mind at this point? During a session I once asked if there is a ritual in preparation for how you prepare to return to you as a partner, parent etc. The supervisee looked taken back, they had never considered this as important.
The consultant who showed deep concern for a patient’s parent reflected on how they share the same fears for their children, they indeed were trying to pacify their own anxiety. We listen to our gut; we get creative – all the luxuries of free thinking and ways of being that professionals such as legal and medical practitioners cannot afford in their day-to-day working lives.
Both professionals function in a setting where overwhelming and unending demands to maintain good standards and meet targets are constant. Therefore, we can see the danger of exposing vulnerability and how it would be considered to have dire consequences. Questioning self and ability leads to imposter syndrome common for doctors and lawyers; this is often brought to supervision along with heightened stress, anxiety and decision fatigue.
Nothing is more important in occupational supervision than the supervisory relationship. It is the foundation of trust that cannot be replicated with another professional who they might encounter in a workplace setting. Trust that they will never have to be compromised in this way allows guards to be dropped. Refreshingly, both medical and legal professionals have recognised there needs to be a shift towards being relatable, preferring to develop warmer, conducive relationships with clients/patients. In occupational supervision we foster a move towards authenticity and freedom in order to connect in meaningful ways, a move towards developing a sense of wellbeing for both professional and their client/patient.
Legal and medical practitioners find occupational supervision to be an oasis of support. They have no fear or apprehension of judgement or compromise. Many have gone so far to say they count the days until their next session.
Lesley Edelstein is an occupational supervisor, psychotherapist, and tutor/trainer